The standard fitting separation for peripheral prisms is 12 mm. Place one 6mm above the pupil, and one 6mm below the pupil. There are 3 situations under which you should consider altering the prism locations
Abnormal Back Vertex Distance
The distance from the front of the eye to the back of the lens is known as the back vertex distance (BVD), and is generally assumed to be 13 mm. The nodal point is assumed to be 7 mm behind that.
For a distance of 20 mm from the nodal point, the separation is 12 mm.
If the total distance from the nodal point to the prisms increases, the distance between the prisms should increase accordingly (0.6mm of additional separation per millimeter of vertex distance.)
If the total distance from the nodal point to the prisms decreases, the distance between the prisms should decrease accordingly (0.6mm of additional separation per millimeter of vertex distance.)
Patients with deep-set eyes or a flatter face may vary dramatically from this standard distance
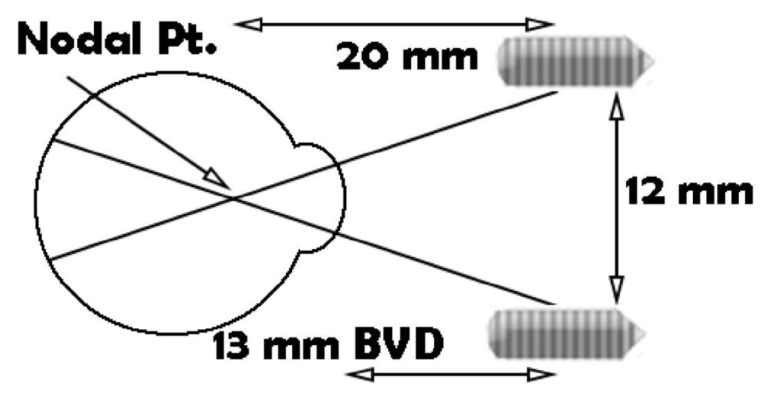
Here’s the formula for calculating the modified separation distance:
(BVD + 7) *0.6
Patient Sensitivity (Or Lack Thereof)
Sometimes patients are bothered by the presence of the prism image in their vision. The natural practitioner reaction to this is to move the prisms temporally. Moving the prisms temporally removes the prisms from the patient’s visual field, rendering them completely ineffective. Alternatively, increasing the separation will move the prisms into a less sensitive area of the patient’s visual field, allowing them to still be effective while being less bothersome.
Conversely, patients might not notice the field enhancement with the standard placement. If that’s the case, reducing the separation will put the prisms in a more sensitive area of the patient’s visual field and make the field expansion more apparent.
Non-Standard Visual Fields
The field loss associated with strokes and head injuries doesn’t always perfectly conform to the pictures we see in textbooks. Many times, a diagnosis of homonymous hemianopsia would have us assume one thing, but the patient has different areas of visual field that may be missing or spared. It’s important to understand the underlying principles of field expansion when treating these patients so we don’t create duplication of visual field, or put prisms in an area that is not useful to the patient. The principles are further laid out in our white paper “Principles in Field Expansion.” While we’re super proud of it, we understand you may not want to read it. If you don’t want to read that, give us a call. We deal with this sort of stuff everyday and love talking about it.